After being a student at middlesex university for 3years I have never felt so independent and competent as a nurse. I am currently in my final year on my final management placement which finishes in 2.5 weeks. Although I look forward to it I still remain nervous, I have worked so hard for this and it has finally come to an end. Today on MAU has been so hectic, I have had 6 patients by myself and although being supervised it feels like I am alone and it feels like I am a nurse. I have been able to manage these patitents by myself and use all my skills that I have gained through the years.
Having spent my final year in Malta I feel like this has helped me alot, it has boosted my confidence, increased my knowledge and the experience has allowed me to grow professionally. However, I feel like as I am not able to use certain skills I obtained in Malta in the UK i.e. taking and reading ABG's, adminsitering IVaa drugs and fluids, cannulating and taking FBC's I feel like I am loosing these skills. I am aware that once I qualify these will come naturally and I will be taking mini courses which will also increase my invovlement in these skills. All the same I am glad I obtained these skills.
What I need to continue to work on I would say is my drugs, I need to familirise myself with common drugs used in the UK. Although time and experience will make increase my drug knowlegde it is something I have identified. If I had to do anything differently within the last 3 years I would pay more attention and do it all over again.
Next Chapter awaits....... :)
MALTA :-)
Thursday, July 21, 2011
Tuesday, June 21, 2011
Health economics in Malta
Malta has a number of free services offered by the health care services, the government also allows free initial treatment (accident and emergency) for the island, a free consultation and a free family Doctor. However, the working populating pays taxes and SOME Maltese people believe the funds are not being used to cater for the needs of the population i.e. health promotion, community services, elderly care, better provisions for a long term care. As a whole the public tend to abuse the health care system because they believe they pay taxes therefore they can choose to call an ambulance as many times as they want or book to see their Doctors whenever they choose etc. Due too these current problems on the Island, the health care system both heirachial and structural which has an effect the nursing process as it can not function as well as it should and influencing continuity of care and support for the patient. Although there is motivation amongst nurses despite lack of statistics and finance there is as the lack of trust in the nursing profession as the health care system is medically dominated by Doctors there is hope that the social economical conditions will imrpove.
Malta has a high increase of ageing population which is not supported by the socio economical conditions, in April 2011 the times of Malta newspaper identified Malta as the only EU country that does have the treatment for osteoporosis, it is said to cost 15euro - 45euro per month. However, if the government brought the treatment in bulk it will cost far less putting a less strain on pensioners who suffer from the disease and saving the tax payer 9,500 euro from a fracture. For further reading go to http://www.timesofmalta.com/articles/view/20110424/local/Malta-only-EU-country-with-no-free-osteoporosis-treatment.362031
Malta has a high increase of ageing population which is not supported by the socio economical conditions, in April 2011 the times of Malta newspaper identified Malta as the only EU country that does have the treatment for osteoporosis, it is said to cost 15euro - 45euro per month. However, if the government brought the treatment in bulk it will cost far less putting a less strain on pensioners who suffer from the disease and saving the tax payer 9,500 euro from a fracture. For further reading go to http://www.timesofmalta.com/articles/view/20110424/local/Malta-only-EU-country-with-no-free-osteoporosis-treatment.362031
Nursing and medical care between ITU & Accident and Emergency
Intensive care is exactly how it sounds, its intensive and A&E worked at fast pace. In intensive care the medical staff included as Anaesthetist (Consultant, SpR, SHO), Pharmacist and the Nursing Officer. Medical alliances that were on the unit included ECG technicians, physio therapist and nursing assistance. Every month there were a turn over of Consultants and Pharmacists, every morning they would each do a around and consider the plan, observe changes and what needs to be done. If a drug was not ideal for a patient then and there, there pharmacists could change the particular drug. The nursing officer would also contribute and identify any problems that had been handed over or documented.
Every nurse was allocated one patient and had to care for them throughout the shift unlike A&E whereby staff were allocated to an area whether it be majors, minors, triage, resus or paediatrics. They received verbal handover in the staff room, then by the bed side, which was given by the previous nurse who also would identify any outstanding things that needed to be done for the patient i.e. X-ray, scan etc. The staff now on duty would read through the patients notes, then wash the patient, take vitals signs and administer medications. Patients were usually on intravenous medication and fluids. Common drugs included Propofol (sedation), Tacurium (muscle relaxant) and Inotropic therapy such as Dobutamine and Adrenalin and Nor-Adrenaline (vasoconstrictors). Every intervention was documents systematically using the nursing process and assessments. The nursing staff there had a close team which I think is not only in the best interest of the staff but also in the best interest of the patients. These patients usually suffered from trauma, shock, multi organ failure or severe respiratory failure. They were visited by their families who prayed for them and some just stood in silence. This placement I must say was touching as there was so many ethical issues to deal with, it made me view life in a different way and I can say was a major learning curve for me.
The accident and emergency it was very much unlike ITU, it was at a fast pace, it had a number of people in every coner and unlike ITU wereby all the patients were sedated or in a coma patients spoke to you. I felt more included when providing care for patients and the day-day routine was far different than ITU. In A&E there was a handover every morning which students including myself never attended to or was invited to. Usually it was the nurses coming on which attending the hand over, there was no structure in the handover it seemed because those that were allocated in resus for an example still listened in the handover but seen as this was mostly in Maltese I could be wrong. In the day, we usually stocked up the trolley, the person allocated to triage would go straight there and the one allocated in resus would stock the resus rooms up. The A&E department also had a control room where calls came in for ambulances, in the mornings there was someone also allocated to the control room. The department received all sorts of injures, all sorts of people and all types of calls. Common injuries and illnesses that came through the department included, muscle skeletal injuries from falls, trauma from motor vehicle accidents and road traffic accidents (MVA's and RTA's) and medical emergencies such as Shock, CVA, cardiac arrests etc. The best part of this A&E was that I was able to do things I would not have ever been given the chance to do in the UK, such as ride on an ambulance to a scene, take arterial blood gasses, cannulation and give IV drugs (under supervision).
Patients that came into A&E via ambulance were either put on on high priority or in the resuscitation room, those that came through triage unless was an emergency were made seated until it was their turn to be seen, unlike the UK were we used the Manchester triage system there was nothing like that in place it was more of a 'first come first served' system which could have put ill patients in immediate harm. Some patients waited so long in the department that they would leave and I believe the system needs to be changes for the grater good. Staff in the department included A&E Dr's, nurses, nursing assistants and cleaners. Although, specialist were some times called, during the time I was there a nutritionist, a psychologist, a surgeon and an anaesthetist were called out for their speciality. I recall on a number of transfer's to X-ray's or CT scan's an anaesthetist accompanied the patient and nursing staff. At the time of this placement was when people from Libya were cast of the country due to civil war, in turn, we had patients who came of the boat from Libya and were cared for in the A&E department. These people felt traumatised and were so please and thankful for every intervention taken out for them. During this placement at times I noticed the Maltese patients pointing and making remarks which felt quite odd. A&E was an interesting place as everything came through the door, although some people abused the services it was an amazing experience for me.
Every nurse was allocated one patient and had to care for them throughout the shift unlike A&E whereby staff were allocated to an area whether it be majors, minors, triage, resus or paediatrics. They received verbal handover in the staff room, then by the bed side, which was given by the previous nurse who also would identify any outstanding things that needed to be done for the patient i.e. X-ray, scan etc. The staff now on duty would read through the patients notes, then wash the patient, take vitals signs and administer medications. Patients were usually on intravenous medication and fluids. Common drugs included Propofol (sedation), Tacurium (muscle relaxant) and Inotropic therapy such as Dobutamine and Adrenalin and Nor-Adrenaline (vasoconstrictors). Every intervention was documents systematically using the nursing process and assessments. The nursing staff there had a close team which I think is not only in the best interest of the staff but also in the best interest of the patients. These patients usually suffered from trauma, shock, multi organ failure or severe respiratory failure. They were visited by their families who prayed for them and some just stood in silence. This placement I must say was touching as there was so many ethical issues to deal with, it made me view life in a different way and I can say was a major learning curve for me.
The accident and emergency it was very much unlike ITU, it was at a fast pace, it had a number of people in every coner and unlike ITU wereby all the patients were sedated or in a coma patients spoke to you. I felt more included when providing care for patients and the day-day routine was far different than ITU. In A&E there was a handover every morning which students including myself never attended to or was invited to. Usually it was the nurses coming on which attending the hand over, there was no structure in the handover it seemed because those that were allocated in resus for an example still listened in the handover but seen as this was mostly in Maltese I could be wrong. In the day, we usually stocked up the trolley, the person allocated to triage would go straight there and the one allocated in resus would stock the resus rooms up. The A&E department also had a control room where calls came in for ambulances, in the mornings there was someone also allocated to the control room. The department received all sorts of injures, all sorts of people and all types of calls. Common injuries and illnesses that came through the department included, muscle skeletal injuries from falls, trauma from motor vehicle accidents and road traffic accidents (MVA's and RTA's) and medical emergencies such as Shock, CVA, cardiac arrests etc. The best part of this A&E was that I was able to do things I would not have ever been given the chance to do in the UK, such as ride on an ambulance to a scene, take arterial blood gasses, cannulation and give IV drugs (under supervision).
Patients that came into A&E via ambulance were either put on on high priority or in the resuscitation room, those that came through triage unless was an emergency were made seated until it was their turn to be seen, unlike the UK were we used the Manchester triage system there was nothing like that in place it was more of a 'first come first served' system which could have put ill patients in immediate harm. Some patients waited so long in the department that they would leave and I believe the system needs to be changes for the grater good. Staff in the department included A&E Dr's, nurses, nursing assistants and cleaners. Although, specialist were some times called, during the time I was there a nutritionist, a psychologist, a surgeon and an anaesthetist were called out for their speciality. I recall on a number of transfer's to X-ray's or CT scan's an anaesthetist accompanied the patient and nursing staff. At the time of this placement was when people from Libya were cast of the country due to civil war, in turn, we had patients who came of the boat from Libya and were cared for in the A&E department. These people felt traumatised and were so please and thankful for every intervention taken out for them. During this placement at times I noticed the Maltese patients pointing and making remarks which felt quite odd. A&E was an interesting place as everything came through the door, although some people abused the services it was an amazing experience for me.
CULTURAL DIFFERENCES......LONDON & MALTA
Health promotion is a process of enabling individuals to increase control of their own health in order to improve it (WHO, 2011). The advantages of health promotion is that it moves from a the focus of individual behaviour and moves to a wide range of social and environmental interventions. In the UK, health promotion is consistent, extensive and vital to the nation. Due to the fact that the UK has a population of 59 million people who have different lifestyles, cultures and ethnic groups this brings out issues and the aim of health promotion is to identify these issues firstly as issues and tackle them. In the UK we have a number of organisations such as Change4Life who promote healthy eating, the British safety council which tackle accidents and Fast forward which aim to prevent alcohol and tobacco abuse. These are just few I have mentioned, they come in all sorts of charities, councils, bodies organisations and volunteers, they have constant adverts, gatherings, meetings, leaflets and aim to make the nation a better place. However in Malta there isn't so many, there is a lack of provisions for health promotion in Malta, although health promotion is gradually improving and will eventually improve over the years it lacks continuity and community support. SOME Maltese people are not willing to take care of there health until they are unwell, they need education in terms of health promotion. Furthermore, other countries contribute and also implement health promotion but it is not as big in comparison to the UK. Having said that, the Maltese are becoming more Westernise and are becoming more aware of the issues they face such as obesity, smoking, alcohol abuse etc. When auditing the effectiveness of health promotion, little is done to enhance the effectiveness or implement change or strategies to reach and educate the public.
http://www.who.int/topics/health_promotion/en/[Accessed 21.06.11]
Sports
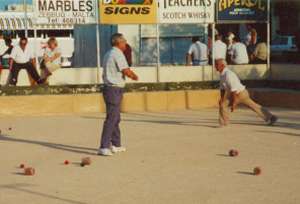
The Maltese are known for their underwater sports, scuba diving, swimming, weights, bocci, water polo, tennis, horse racing and football. Football is Malta's national sport, as the UK. Bocci, is a local game played on a sand with three players. Water polo and other water sports are usually played in summer months and horse racing, which is the longest traditional sport in Malta has been around for many years and is taken very seriously.
Here is a picture of the game BOCCI being played by locals.
However, in the UK the biggest sports is football, cricket and rugby. These matches are haled in big stadiums and are also taken very seriously. Personally I'm a Manchester United fan.
Leisure Facilities
The Maltese are really laid back, they know how to have a good time and unwind after a hard day at work. In Malta there are tones of night clubs,open bars, restaurants and sea front night life seen. However, in London we tend to use what we call the 'pub' it's a place used to unwind after work and used to binged drink. Pubs are rituals for some and are seen in common T.V series such as EastEnders. There is also a place called the West end, which has 500,000 people entertained every weekday and weekend.
Friday, June 17, 2011
The Maltese word and phrases (1st and 2nd Semester)
The Maltese language is consist of Maltese and English as their second dialect. Maltese has a Semitic tongue and has evolved from the earlier Semitic language of the Assyrian's and the Babylonians, which stretched westwards from the Middle East till the shores of Palestine in the Eastern Mediterranean. Unlike other Semitic languages, Maltese is written in the Latin alphabet, but with the addition of special characters to accommodate certain Semitic sounds. There is much in the Maltese language today that is not semitic due to the immeasurable romance and influence from the succession of the Southern European rulers through the ages. However, the language has a special glottal sound for the letter "Q" which resembles neither the Arabic, nor the European sounds for its equivalent (which are more akin to our 'k' sound), but is rather like the sound produced by a 'silent cough'. Another thing I found evident is that over the years due to the fact Malta has been dominated over by different leaders they all influenced the language and by adding their own such as 'Bonjourno' taken from the French which means 'Good morning' or 'Ciao' from the Italian's which means 'Goodbye'.
http://www.my malta.com/interesting/MalteseLanguage [Accessed 19th May 2011].
Durning the first in my ITU placement there were only a few words/phrases used to patients and some families did not want to interact due to their current state however, I learnt to say:
'PUT YOUR HANDS DOWN' which is 'NIZZEL IDEJK, JEKK JOGGHBOK'. I used this saying in ITU when some of the patients where not adhering to their non-invasive ventilation (NIV) and they would often have their hands to the NIV trying to take it off as it is uncomfortable.
'BREATH IN AND OUT' which is 'HU NIFS IL-GEWWA U L-BGRRG'. This was often used when saturations where low for no apparent reason, I would ask the conscious patient to sit up right and breath in and out.
'MY NAME IS ALEXIS' which is 'JEIN JL'SMINI ALEXIS'. This was used when introducing myself before taking out any form of care for the patient.
'GOODBYE' which is 'CAW/SAHHA' When leaving the patient or even leaving the ward, I would often day this to my colleagues.
In the second semester during my Accident and Emergency placement I was able to learn more words and use more phrases and I remember saying it to a few patients or relatives and they were impressed. I learnt to say:
'COUGH FOR ME PLEASE' which is 'ISSOL, JEKK JOGGHBOK'. This was used when I wanted to listen to the patients breathing sounds during client assessment.
'WHAT BEINGS YOU TO EMERGENCY' which is GHALIER GEJT I-EMERGNIZA'. This was used in triage mainly, before caring out the next assessment.
'YOU WILL BE SEEN SOON' which is 'DAQT JIGU JARAWK'. This was used in A&E as some patients became restless and anxious and asked when they will be seen.
'THIS IS YOUR MEDICATION' which is 'DH HI I-MEDICINA TIEGHEK'. Under supervision I gave medication to patients and this was used to express it.
'RELAX FOR ME PLEASE' which is 'IRRILASSA, JEKK JORHGBOK'. When taking respiration rate and other procedures such as taking bloods or putting in a nasogastric tube, I often would tell the patient to relax.
'TRY NOT TO MOVE' which is 'PROVA TICAQLAQX'. This was often used when cannula-ting patients in the A&E department.
http://www.my malta.com/interesting/MalteseLanguage [Accessed 19th May 2011].
Durning the first in my ITU placement there were only a few words/phrases used to patients and some families did not want to interact due to their current state however, I learnt to say:
'PUT YOUR HANDS DOWN' which is 'NIZZEL IDEJK, JEKK JOGGHBOK'. I used this saying in ITU when some of the patients where not adhering to their non-invasive ventilation (NIV) and they would often have their hands to the NIV trying to take it off as it is uncomfortable.
'BREATH IN AND OUT' which is 'HU NIFS IL-GEWWA U L-BGRRG'. This was often used when saturations where low for no apparent reason, I would ask the conscious patient to sit up right and breath in and out.
'MY NAME IS ALEXIS' which is 'JEIN JL'SMINI ALEXIS'. This was used when introducing myself before taking out any form of care for the patient.
'GOODBYE' which is 'CAW/SAHHA' When leaving the patient or even leaving the ward, I would often day this to my colleagues.
In the second semester during my Accident and Emergency placement I was able to learn more words and use more phrases and I remember saying it to a few patients or relatives and they were impressed. I learnt to say:
'COUGH FOR ME PLEASE' which is 'ISSOL, JEKK JOGGHBOK'. This was used when I wanted to listen to the patients breathing sounds during client assessment.
'WHAT BEINGS YOU TO EMERGENCY' which is GHALIER GEJT I-EMERGNIZA'. This was used in triage mainly, before caring out the next assessment.
'YOU WILL BE SEEN SOON' which is 'DAQT JIGU JARAWK'. This was used in A&E as some patients became restless and anxious and asked when they will be seen.
'THIS IS YOUR MEDICATION' which is 'DH HI I-MEDICINA TIEGHEK'. Under supervision I gave medication to patients and this was used to express it.
'RELAX FOR ME PLEASE' which is 'IRRILASSA, JEKK JORHGBOK'. When taking respiration rate and other procedures such as taking bloods or putting in a nasogastric tube, I often would tell the patient to relax.
'TRY NOT TO MOVE' which is 'PROVA TICAQLAQX'. This was often used when cannula-ting patients in the A&E department.
These may not be the exact spelling......
......these are the words learnt so far :)
My experience of being a student on my first placement...
My first placement in Malta was in the Intensive Care Unit (ITU). ITU is a unit that care for patients with life-threatening conditions whom need constant care, close monitoring and support form equipment and medication to keep normal body functions going. The unit uses specialised monitoring and treatment equipment and staff are highly trained in caring for the most severely ill patients http://www.ics.ac.uk/patients___relatives/what_is_intensive_care_).
As usual going into a new setting is nerve racking, as you never know what to expect let alone in a a different country, which have a different language, a different way of living and a different way of caring for people. As a matter of a fact I assure you, it was more than I expected. When I first arrived on ITU the first thing I noticed was the wires and technical machines and equipment attached to patients, I was then introduced to the Nursing Officer (a title we do not have in the UK) and was given a day that I was expected to come in and meet my mentor. On my first day my mentor was not around however, I was allocated to another staff to work with. This member of staff showed me around, introduced me to other staff and we began the shift after handover. It was my first time in the ITU as did not know what to expect. Not long after I discovered that patients that came into ITU was either semi-concisions,sedated or in a coma following a trauma, multiple organ failure or needed respiratory support.

At the time of this placement, I was also undertaking a class on Critical care with Maltese students. Taking the class was beneficial as ITU as a placement I had never been, it helped put theory into practice, it allowed me to visualise evidence based practice and reflective learning. Taking the class also boost my confidence and allowed me to practice effectively. The topics covered in class included caring for a patient in shock, infection prevention and control, care of the patient with burns, haemodynamic monitoring, electrocardiogram monitoring, arterial blood gasses monitoring, pulmonary oedema, airway management, mechanical ventilation and caring for the head injured patient. Below is a picture of the lecture and my colleagues:

During the placement I was able to take participate in taking arterial blood gasses, manage invasive ventilation, monitor vital signs, practice documentation, provide care for the critically ill (including, skin care, oral care, IV, SC and IM medication and many others), assist families, attend other investigations such as CT scans, X-rays and MRI scans. I learnt so in both class and in practice that I would have never imagined and will always be with me. I felt as part of the team, I listened to discussion on patients, ethical issues that had to be dealt with in-relation to dying with dignity, removing life support etc. I also got the chance to spend a day in critical areas such as the renal unit, the critical cardiac unit, the neonatal and paediatric unit and the burns and plastic unit. Below is a picture of me caring for a sick patient under supervision: The intensive care unit involved working along side, Doctors (Consultants, Registers, Specialist House Officers), Anaesthetists , Pharmacists, Nursing Officers and Nursing staff. There were also medical allied staff including physiotherapist, ECG technicians and radiotherapist who saw patients regularly. This shows that there were a number of different health professionals in the multi disciplinary team who worked well and closely together.
The intensive care unit involved working along side, Doctors (Consultants, Registers, Specialist House Officers), Anaesthetists , Pharmacists, Nursing Officers and Nursing staff. There were also medical allied staff including physiotherapist, ECG technicians and radiotherapist who saw patients regularly. This shows that there were a number of different health professionals in the multi disciplinary team who worked well and closely together.
 The intensive care unit involved working along side, Doctors (Consultants, Registers, Specialist House Officers), Anaesthetists , Pharmacists, Nursing Officers and Nursing staff. There were also medical allied staff including physiotherapist, ECG technicians and radiotherapist who saw patients regularly. This shows that there were a number of different health professionals in the multi disciplinary team who worked well and closely together.
The intensive care unit involved working along side, Doctors (Consultants, Registers, Specialist House Officers), Anaesthetists , Pharmacists, Nursing Officers and Nursing staff. There were also medical allied staff including physiotherapist, ECG technicians and radiotherapist who saw patients regularly. This shows that there were a number of different health professionals in the multi disciplinary team who worked well and closely together.During my time in ITU I was also given the chance to visit the critical cardiac unit (CCU), the renal unit, the burns and plastic unit and the neonatal and paediatric unit (NPICU). The cardiac unit is a nurse led unit, it has 6 beds and on the day of the visit it had two critical patients. They were both post op; these patients usually come in following a general aesthesia cardiac operation such as a bypass, valve replacement, a heart transplant any many more. With these patients they usually came from ITU with a propofol infusion, an analgesia infusion, a urinary catheter, a drain and mechanical ventilation via an ETT. The nurses are usually ITU trained and are able to manage such equipment. These patients are monitored constantly; they have ECG leads, an arterial line, and central venous line. Fluid for maintenance, a cardiac output machine, pulse oximetry, saturation probe and a temperature probe. On one of the patients was a pulmonary arterial line which measures the pressure (PAP) on the right side of the heart and on the other patient was a machine called the inter aortic balloon pump, is a mechanical device that decrease the myocardial oxygen demand while at the same time increase cardiac output. It is used commonly for previous suffers of a M.I and post bypass, it has its risks however; it lowers the risk of an embolism. Other major complications associated with cardiac problems are stroke and kidney problems. These can hinder us to from certain interventions which can be beneficial to the patient e.g. If a patient who has CHF develop kidney problems, the heart will then increase its work load causing further problems or if a patient has too low of a blood pressure and has renal failure, dialysis which will ultimately benefit the patients may not be taken into consideration. Thus, depending on the patient the appropriate care is given and what is best for the patient will be at the heart of any decision. Patients with heart conditions usually have other health problems such as dyslipidemia, diabetes, asthma, obesity etc. They are advised to take care of their diet, exercise and be compliant with medication. Over all, this placement what short yet interesting.
The NPICU has always been an area which has always been difficult for me to work and as I have a 'soft spot' for children and seeing them unwell is extremely hard for me. This NPICU took babies from birth to 1year old, these babies were either premature, had respiration disorders, problems during birth, chromosomes problems, infections, syndromes or were sometimes admitted for close monitoring. There was also an outpatient which parents brought their babies for treatment and to assess their progress. The inpatient babies were washed, feed and treatment was given in the morning. They were so tiny and cute. The babies were cared for in a machine known as an incubator, the incubator was humidified to retain heat, minimise infection, and protect the babies and kept them warm. Some of these babies were critical and had to be intubated for ventilation. Like adults these babies had where regularly monitored, their blood pressure, pulse, saturation were checked hourly. Some also had an umbilical arterial blood pressure (IABP) measured which bloods were taken from however, unlike the adult ABG’s their dead space of two millilitres blood was given back to them. There was this particular baby who was on a ventilator, born at 28 weeks but look liked 200 pounds, her mother was an immigrant and was 15 years old. The baby was very unwell and it seemed there was not much more that could be done for her. A week later I went back to see the baby and she was still there fighting for her life. She was said to be doing much better and had gain a bit of weight, I cried with joy. NPICU is my weakest emotional point which needs working on, however my time there was well spent.
Another place I visited was the renal unit, the renal unit had a critical outpatient setting for patients with renal failure. This unit had different departments for different types of dialysis. The functions of kidneys are vital, they eliminate water, wastes and waste products such as excess potassium and sodium, creatin and urea. They produce vitamin D, red blood cells in the bone marrow and controls blood pressure via homeostasis. The red blood cells maintain our haemoglobin and if its low erythropoietin (EPO) is given. EPO is an artificial hormone. There are three kinds of accesses for dialysis; these are the tenchkopf via the peritoneum which is used in CAPD and APD (these will be explained further) and then there is the fistula (upper limbs), graft (an artificial tube), permcath (femoral, subclavian or jugular veins) and vascath (the same as the permcath but temporally). These last four are used for haemodialysis where their patients come into the unit 2-3 times a week for the haemodialysis machine to ‘clean’ their blood. The haemodialysis machine is connected via an artery and a vein. The needle is inserted into the access by the arterial line which is always away from the heart and then the venous line which is towards the heart. The arterial blood is usually red and thick whilst the venous line is usually dark, the blood is taken from the arterial line through the machine filtered and heparinised and returned via the venous line. The machine usually has heparin, saline, water for osmosis, a filter and a chamber which clotting can be observed. The procedure usually last for 4 hours and BP is measured during the dialysis. The CAPD/APD is used in independent patients whereby a bag is attached to remove the toxins and a high concentration of dextrose is administered, this usually takes up to twenty minutes to achieve. It is done up to twice a day and an APD machine all night. The reason of choice for these patients are based on their knowledge and understanding, an assessment, venous access, patients desire or choice, lifestyle and access availability such as veins. This placement was very informative as I had never worked in renal but had dealt with renal patients and had never fully understood the concept. It made me feel like some of us take things for granted because they are restricted to what they eat, drink and do. If I could do anything differently I would have like a longer placement. Having visited these different areas I gained incite to as to what they do on a day to day bases and dealt with my emotions when working with babies and young children.
Overall, I was on the ITU placement for approximately ten weeks and after six weeks I remember feeling confident as day in and day out and no two days were the same however, I saw young people, vulnerable people and older adults come in and some did not survive. Some were taken of life support because all that could have been done had been done for these patients. This mad me feel sad, it made me think it could happen to any one of us and our families. After 10 weeks on there it felt daunting and stressful having to care for extremely sick people. What I kept thinking was this could be me, it made me miss my family and not want to take life for granted. However, if I had the chance to take another ITU placement, I would grasp it without a thought and make the most out of it. What I would have done is grasped on much more as I possibly can.This placement taught me a lot, medically, personally and spiritually and for that I will always be grateful.
My impression of the typical Maltese patient and their family.
Although all patients are vulnerable the Maltese patient can be very demanding. The Maltese are very health concious when unwell, the tend to contact their family Doctor and frequently contact specialist for minor injuries and illnesses and call out for ambulances for the slightest things. In spite of their reliance on health services their religious tradition often plays a major role in response to injury and illness commonly in the older adults and in chronic/incurable situation. In most cases the Maltese patient and rely on Doctors a lot, they diminish the use of community services and the nursing profession due to lack of trust. They tend to abuse available facilities e.g. a dying cancer patient will be encouraged to die at home as it will benefit the patient and the can die with dignity a Maltese family will opt for the patient to die in a hospital, if offered one pair gloves the will want a box etc. However, when a illness occurs the family support is strong, the help each other get through hard times, they show up for the ill patient and provide them with prayer, love and support which I guess is always good for a patient to have.
(Picture to be loaded)
I found it easier to communicate with patients and their in A&E than ITU for the obvious reasons. The patients and families that I came across dealt with their illness/injury in different ways, some where demanding, some where angry and going through the stages of grief, some were grateful for assisting and caring for them and others just needed support and someone to listen to. As a foreigner I wasn't always welcomed with open arms however, I did as much as I could to be involved, to answer questions and used my basic Maltese language I learnt to communicate with patients I cared for.
(Picture to be loaded)
I found it easier to communicate with patients and their in A&E than ITU for the obvious reasons. The patients and families that I came across dealt with their illness/injury in different ways, some where demanding, some where angry and going through the stages of grief, some were grateful for assisting and caring for them and others just needed support and someone to listen to. As a foreigner I wasn't always welcomed with open arms however, I did as much as I could to be involved, to answer questions and used my basic Maltese language I learnt to communicate with patients I cared for.
Subscribe to:
Comments (Atom)